
At MWDN, we’ve spent over 20 years helping healthcare companies, like NiCas, find the right tech talent, and along the way, we’ve learned a lot about the unique demands of the medical industry. One area that’s rapidly evolving and often misunderstood is medical coding software. What types are out there? What features actually matter? And when does it make sense to build your own in-house solution? In this article, we’ll unpack it all.
Content:
- What is medical coding, and why is it essential in 2025?
- What businesses need medical coding?
- Three types of medical coding
- How to choose the right encoder software
- Prices of medical coding encoder software
- Things you need to create medical coding in-house
What is medical coding?
Medical coding involves converting a patient’s medical history into standardized code sets, so the information can be used and shared. In practice, coders read the clinical notes and assign codes such as the International Classification of Diseases (ICD-10-CM) for diagnoses and hospital procedures, and Current Procedural Terminology (CPT) or similar code sets for professional services and supplies.
These codes do far more than create a bill: They affect insurance payment and authorizations, feed quality and safety programs, support public-health reporting, and make data usable across EHRs and analytics tools.
The field is often misunderstood, though! There are three reasons for that.
- First, many people think coding is just “billing” or data entry; in reality, it is a clinical abstraction task that requires deep knowledge of guidelines, insurer policies, and medical reasoning.
- Second, the rules change frequently. There are regular quarterly edits and yearly code updates, so last year’s answer may be wrong today.
- Third, medical notes are not always clear, which means coders must ask clinicians for clarification, and those details directly affect both payment and quality metrics.
Put simply, coding is the hinge between clinical reality and everything the health system does with that reality: care coordination, reporting, compliance, and getting paid. When coding is right, organizations reduce denials, reflect true patient complexity, and make better decisions; when it’s wrong, costs rise, and the data can’t be trusted.
What businesses need medical coding software programs?
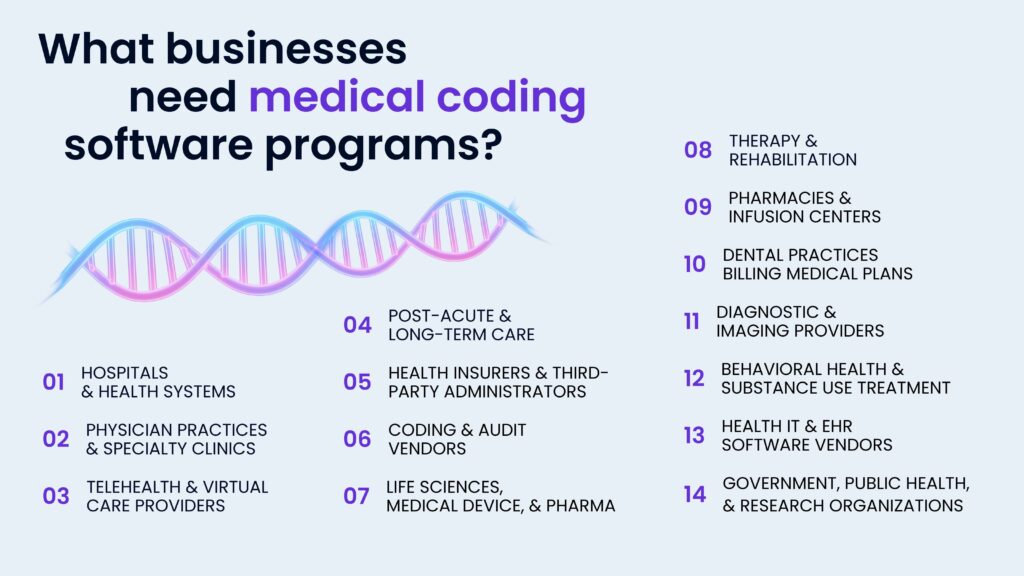
Shortly speaking, if a business does anything with healthcare billing, tracks quality, or analyzes care, it needs medical coding. Among them are:
- Hospitals and health systems. They code diagnoses and procedures to drive payment, risk, and quality metrics, while high audit exposure makes accuracy essential.
- Physician practices and specialty clinics. They translate visits and procedures into billable services and document complexity for contracts and risk programs.
- Telehealth and virtual care providers. They apply correct codes, modifiers, and place-of-service rules for video, phone, and remote monitoring so payers reimburse consistently.
- Diagnostic and imaging providers. They use procedure and diagnosis codes to prove medical necessity, support prior authorization, and meet reporting requirements.
- Therapy and rehabilitation. They capture units, frequency, and documented progress to support coverage decisions and reduce denials.
- Post-acute and long-term care. They align clinical documentation improvement with required assessments and codes that determine payment and case mix.
- Behavioral health and substance use treatment. They code psychotherapy, evaluations, and treatment episodes accurately to comply with payer rules and privacy constraints.
- Pharmacies and infusion centers. They bill medical-benefit drugs and equipment using the correct product and administration codes, often with strict prior authorization.
- Dental practices billing medical plans. They convert applicable services to medical codes when coverage shifts from dental to medical insurance.
- Health insurers and third-party administrators. They use coding to adjudicate claims, adjust risk, detect fraud/waste/abuse, and manage networks and benefits.
- Coding and audit vendors. They provide outsourced coding, audits, HCC capture, and submissions to clinical registries and quality programs.
- Health IT and EHR software vendors. They embed coding rules, edits, and computer-assisted coding into workflows to improve speed and accuracy.
- Life sciences, medical device, and pharma. They support reimbursement strategy, market access, and adverse-event/diagnosis coding in studies and real-world evidence.
- Government, public health, and research organizations. They rely on coded data for surveillance, registries, policy analysis, and population-health reporting.
Three types of medical coding
Medical-coding software generally falls into three categories:
- Rules-based/traditional encoders that apply official code sets and decision logic,
- NLP/AI-powered encoders that read clinical notes and suggest codes for human validation, and
- EHR integration (often cloud) encoders that embed coding directly into documentation and claims workflows.
They address different needs, like consistency and compliance, speed and capture, and many modern tools blend elements of all three. Let’s examine each type in detail, including use cases, strengths, and common pitfalls.
Rules-based / traditional encoder software
Rules-based encoders guide human coders through official code sets and decision trees to assign ICD-10 diagnosis/procedure codes and CPT/HCPCS codes consistently. They surface edits, references, and grouping/reimbursement logic so coders can justify choices and pass audits. Tools of this type emphasize explainability and adherence to coding guidelines over automation.
Core features include:
- Coding pathways and decision logic that walk coders through to complete, compliant code sets.
- Authoritative code look-up across ICD-10-CM/PCS, CPT, and HCPCS with lay descriptions and continual code updates.
- Edits, policies, and crosswalks, and coding tips to reduce denials.
- Grouping/reimbursement views to see the financial implications of code choices.
- Audit trail and content citations to support compliance reviews.
- Deployment options from web-based access to cloud delivery and integration with rev-cycle tools.
This kind of software is used in high-scrutiny environments, like hospitals, where explainability and guideline fidelity are critical, for training and standardization for teams that need consistent outcomes across coders and locations. And in complex cases where human judgment is essential, and AI suggestions aren’t trusted without clear source logic.

NLP/AI-powered encoder software
NLP/AI encoders read clinical notes and extract concepts, like diagnoses, procedures, and tests. Then map them to suggested codes for coder review or, in some products, fully autonomous submission for selected encounter types. These systems combine natural-language processing with clinical rules and reimbursement logic to speed throughput while keeping an evidence trail for audits. Examples include AI modules inside established CAC platforms and newer “autonomous coding” engines.
It is used in high-volume specialties, like emergency departments or primary care, where automation measurably reduces backlog, denials, and turnaround time. It is also used in case of staffing constraints and cost-reduction initiatives where partial or full automation maintains throughput without adding headcount and with mixed workflows that benefit from coder-in-the-loop review on complex cases and automation on routine ones.
Many deployments blend categories: traditional encoder systems + AI suggestions for complex charts, and an autonomous engine for routine encounters. The deciding factors are volume, case complexity, audit requirements, and the need for direct-to-bill automation vs. coder-validated workflows.
Integrated EHR/PM system encoders and cloud-based solutions
These are coding and charge-capture tools built directly into an EHR or practice-management system, often delivered in the cloud, so coders and clinicians can assign diagnoses/procedures, run edits, and create claims without leaving the core workflow.
Key features:
- Embedded charge capture and coding rules (ICD-10, CPT/HCPCS) with edit checks/scrubbing before claims submission, reducing rework and denials.
- Cloud delivery and continuous updates to payer rules and coding content, plus direct handoffs to billing/RCM modules.
- Coder or service assist inside the EHR/PM (e.g., in-platform coding teams or add-on services) for backlogs and consistency.
Prices of medical coding encoder software
Below is a practical view of pricing models for medical-coding encoder software, plus real price points where different types of medical coding encoder software available on the market today publish them.
Per-user subscriptions are typical for rules-based online encoders used by coders and auditors. The costs vary from the standard package $299.95/user/yr, to the expert $999.95 (list prices shown on Optum’s product pages).
Per-encounter pricing is common for NLP/AI platforms that code charts automatically, often with “pay only when successfully coded” terms. Vendors often lead with outcomes: Fathom cites 90%–96%+ automation rates; Nym case studies cite 50% cost reduction per chart; CodaMetrix markets about 30% lower coding cost. So, there are usually just performance claims, not pricing as is.
Some platforms charge per transaction beyond an included bundle. For example, Find-A-Code includes 50 claim-scrubs/month; extra scrubs are tiered ($0.15 down to $0.05 per claim as volume grows).
How to choose the right encoder software?
- Define your use cases and scope
- Decide your “engine” type
- Insist on evidence and content depth
- Fit it into your workflow (don’t bolt it on)
- Set automation guardrails and governance
- Measure the right outcomes
- Security, privacy, and compliance
- Usability and change management
- Total cost of ownership and ROI
- Prove it before you buy
- Plan the rollout and what happens next
But, here’s one more thought: given your requirements, content dependencies, and integration needs, maybe it is wiser to build your own encoder instead of buying an off-the-shelf product?
Things and people you need to create medical coding in-house

If you plan to create your own encoder programs, you’ll need a cross-functional team that covers product, domain expertise, engineering, data, security, and operations. Here’s who you will need.
Product and domain
- Product Manager (health IT)
- Clinical Coding SME (AHIMA/AAPC)
- CDI Specialist / Clinical Informaticist
- Reimbursement and Payer Policy Analyst
- Terminology/Ontology Engineer
- Compliance and Privacy Officer
Software engineering
- Tech Lead / Architect: chooses architecture, scalability, and integration patterns.
- Backend Engineers: build coding services, rules engines, grouping logic, audit logging, and APIs.
- Frontend Engineers (Web): create coder worklists, evidence views, dashboards, and admin consoles.
- Integration Engineers: implement HL7 v2/FHIR, X12 (837/835), and EHR/PM connections (Epic/Oracle Health/others).
- Data Engineers: build ETL/ELT pipelines, reference content imports, and payer rules feeds.
- DevOps / SRE / Cloud Architect: CI/CD, observability, cost control, HA/DR, infrastructure as code.
- DBA / Data Platform Engineer: indexing, query performance, PHI partitioning, retention policies.
- QA / Test Automation: unit/integration tests, synthetic charts, regression suites for code set updates.
- Security Engineer (AppSec): SSO/IdP, least-privilege access, vulnerability management, secure SDLC.
Customer delivery and support
- Implementation Specialist: EHR/PM hookup, SSO, data flows, and site configuration.
- Customer Support Engineer: triage, issue reproduction, and fix verification with PHI-safe processes.
- Analytics Lead: reporting on denials, first-pass yield, throughput, and coder productivity.
Tooling and prerequisites to plan for
Apart from people, you will also need licenses for code sets/terminologies (e.g., CPT, SNOMED CT, LOINC) and payer policy feeds, access to de-identified charts for testing/training; EHR sandboxes; DRG/groupers as needed, audit logging, consent tracking, and model/content versioning, and formal update calendar for code sets and payer edits, with regression testing before each release.
Or… assemble this team faster with MWDN
Building this capability requires many specialized roles that can be hard and expensive to hire locally (especially in Israel or US). With MWDN, you can staff these roles remotely as a dedicated team or as individual specialists at a significantly lower total cost than local hiring, while keeping your IP and standards intact.
What MWDN provides
- The right roles on demand
- Fast staffing
- Flexible models
- Security and compliance
- Operating cadence that fits you
- Stability: long-term engineer retention so your domain knowledge stays with the team.
If you want to build a healthcare IT company without assembling every role locally, MWDN can put the team together and keep it running so you can focus on product and outcomes.
Book a call to find out more!
Content
- 1 What is medical coding?
- 2 What businesses need medical coding software programs?
- 3 Three types of medical coding
- 4 Prices of medical coding encoder software
- 5 How to choose the right encoder software?
- 6 Things and people you need to create medical coding in-house
- 7 Or… assemble this team faster with MWDN

